TL;DR
- Smoking doubles the risk of dental implant failure
- Quit smoking 2-4 weeks before surgery for better success
- Success rates drop from 90-95% in non-smokers to 80-85% in smokers
- Temporary abstinence can nearly eliminate the risk
Dental Implant Success Rate for Smokers: What the Numbers Reveal
Introduction: A hidden gamble in your smile
Jacob always dreamed of regaining the confidence that came from a full, healthy smile. After losing several teeth to decay, his dentist suggested dental implants - titanium posts surgically anchored into the jaw that look and function much like natural teeth. At their best, implants offer freedom from dentures and a permanent solution to tooth loss. In fact, among non‑smokers, studies show implants succeed 90-95 % of the time. But Jacob hesitated because he was a smoker. His dentist warned that nicotine could threaten the life of his new teeth and that “for smokers, the odds of a dental implant lasting a decade may drop by nearly half.”
That striking warning raises an important question: how much does smoking really affect dental implant success rates? To answer it, we must unpack what “success” means for implants, examine the numbers from large studies, understand why smoking hurts bone healing, and explore how quitting - even temporarily - can tilt the odds back in a patient’s favor.
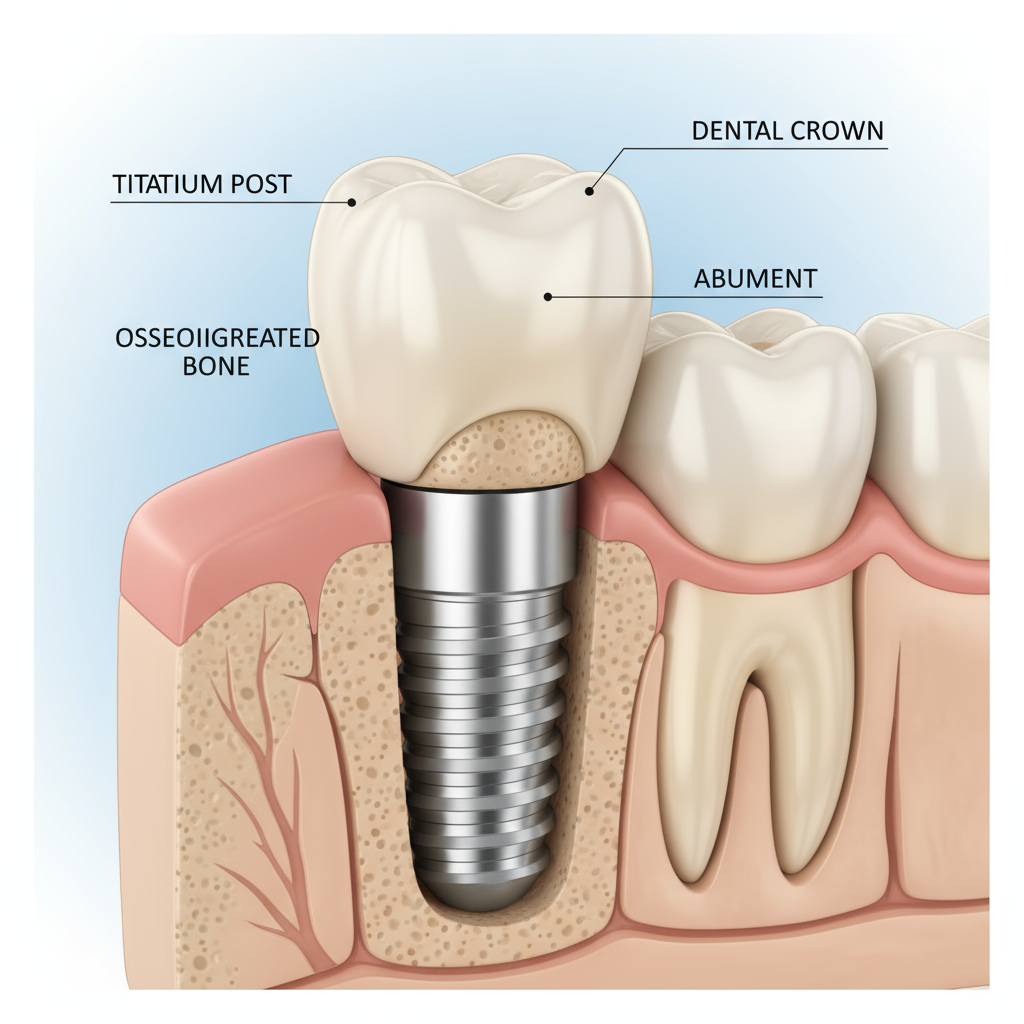 Figure 1: Illustration of a dental implant successfully osseointegrated in healthy bone tissue.
Figure 1: Illustration of a dental implant successfully osseointegrated in healthy bone tissue.
Understanding dental implant success
A dental implant is a small titanium (or titanium‑zirconium) cylinder placed into the jawbone to replace the root of a missing tooth. After placement, the body must grow new bone directly onto the implant surface in a process called osseointegration. Successful osseointegration means the implant becomes firmly anchored and can withstand biting forces. Clinically, implant “success” is judged by several criteria:
- Survival: the implant remains in place without needing removal.
- Stability: no mobility when tested by a dentist.
- Healthy tissues: the surrounding gums show no persistent inflammation or infection (peri‑implantitis) and bone loss around the implant remains minimal (commonly ≤ 1 mm during the first year and < 0.2 mm annually thereafter).
When these conditions are met, implants can function for decades. Large clinical studies report implant survival rates of about 90-95 % in non‑smokers over five to ten years. For example, a long‑term prospective study of 453 implants followed for ten years found patient‑level survival of 82 % and implant‑level survival of 93 % among non‑smokers[1]. Those high success rates have made implants the gold standard for replacing missing teeth.
The numbers: smokers vs. non‑smokers
Multiple systematic reviews and clinical studies consistently report that smoking roughly doubles the risk of dental implant failure. Below are headline figures from recent research:
- A 2021 meta‑analysis pooled data from 292 publications and found that smokers were 2.4 times more likely to experience implant failure (odds ratio = 2.402), meaning a 140 % higher risk compared with non‑smokers[2]. Smokers also experienced 0.58 mm more marginal bone loss around implants than non‑smokers[2].
- In a ten‑year prospective cohort study, smokers had a patient‑level implant survival rate of only 75 % versus 82 % in non‑smokers. At the implant level (each individual implant), survival was 81 % for smokers and 93 % for non‑smokers, a gap of more than ten percentage points[1]. When success was defined stringently - bone loss ≤ 1 mm - 81.2 % of implants in non‑smokers met the threshold compared with 59.7 % in smokers[3].
- The same study found the hazard of implant loss in the upper jaw (maxilla) was 5.64 times higher in smokers than non‑smokers[1]. Smokers also lost more bone (1.9 mm vs. 0.8 mm) around implants[1].
- A 2024 systematic review of long‑term cohort studies reported that failures in smokers were 2.23 times more likely than in non‑smokers[4]. Heavy smokers (10+ cigarettes per day) were 18.3 times more likely to experience implant failure[5], and one large study cited in the review found failure rates of 13.5 % in smokers versus 4.4 % in non‑smokers[5].
- A retrospective analysis of 7,680 implants revealed failure rates of 5.6 % in smokers versus 3.5 % in non‑smokers[6]. The same study noted that patients who quit smoking but underwent implant placement within two years of cessation had a 2.7‑fold higher risk of failure compared with those who waited more than two years[6].
Comparing success rates at a glance
| Outcome | Non‑smokers | Smokers | Evidence |
|---|---|---|---|
| Five-ten‑year survival | ~90-95 % survival | ~80-85 % survival (drops further with heavy smoking) | Meta‑analyses & cohort studies[1][4] |
| Ten‑year patient‑level survival | 82 %[1] | 75 %[1] | Prospective cohort study |
| Ten‑year implant‑level survival | 93 %[1] | 81 %[1] | Prospective cohort study |
| Success (≤ 1 mm bone loss) | 81.2 %[3] | 59.7 %[3] | Prospective cohort study |
| Marginal bone loss | ~0.8 mm after 10 yrs | ~1.9 mm after 10 yrs | Prospective cohort study[1] |
| Odds of failure | Baseline | 2-3× higher | Meta‑analyses[2][4] |
| Heavy smokers (>10 cig/day) | Baseline | Up to 18× higher | Systematic review[5] |
In addition to these large studies, numerous smaller clinical reports tell the same story: smokers lose implants earlier and experience more bone loss and gum inflammation than non‑smokers. Some dental clinics even quote anecdotal figures-such as failure rates climbing from about 1 % in non‑smokers to over 15 % in smokers[7]-though these numbers may exaggerate the difference in a broader population. Still, the trend is clear: nicotine compromises the long‑term success of dental implants.
Why smoking hurts implant success
A hostile environment for bone healing
Dental implants rely on the body’s ability to lay down new bone around the implant surface. Nicotine and other chemicals in tobacco smoke disrupt this delicate process in several ways:
- Reduced blood flow and oxygen: Smoking causes blood vessels to constrict and damages the lining of arteries. During healing, adequate blood flow is essential to deliver oxygen, nutrients and immune cells to the surgical site. In smokers, reduced blood supply slows the formation of new bone and soft tissue.
- Impaired immune response: Tobacco smoke impairs white blood cell function, making it harder for the body to fight infection. Consequently, smokers have a higher risk of postoperative infection, which can cause early implant failure. A retrospective study found that among failed implants in smokers, two of six failures (1.9 % of total implants) were due to infection[8].
- Delayed osseointegration: Nicotine interferes with osteoblasts, the cells responsible for building bone, and stimulates osteoclasts, which break down bone. Studies show smokers experience more than double the marginal bone loss compared with non‑smokers[1].
- Higher risk of peri‑implant disease: Peri‑implant mucositis (gum inflammation) and peri‑implantitis (inflammatory bone loss) are major causes of late implant failure. A 2025 consensus report from the American Academy of Periodontology (AAP) and Academy of Osseointegration (AO) found that smoking significantly affects the mucosal barrier and peri‑implant microbiota and is associated with peri‑implant mucositis (odds ratio 1.47)[9]. For peri‑implantitis, smoking increases risk by roughly 2.27 times[10]. Current or former smokers who quit less than ten years ago are considered high‑risk[11].
One expert likens the effect of smoking on implants to “trying to plant a tree in soil starved of water and nutrients.” Without proper blood flow and immune support, the implant may never fully integrate or may succumb to infection and bone loss over time.
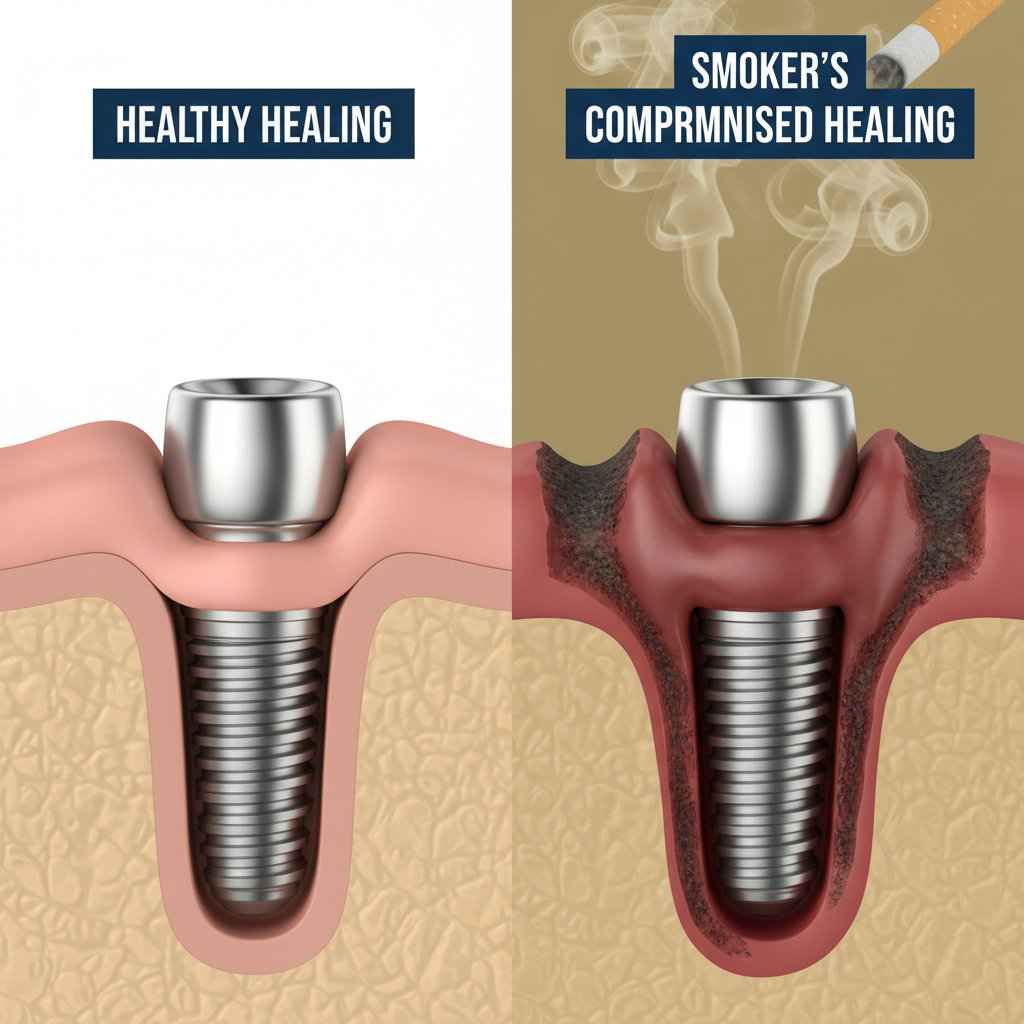 Figure 2: Comparison showing healthy osseointegration (left) versus compromised healing with bone loss in smokers (right).
Figure 2: Comparison showing healthy osseointegration (left) versus compromised healing with bone loss in smokers (right).
Does quitting help? Evidence from cessation studies
The good news is that quitting or even temporarily abstaining from smoking can substantially improve implant outcomes. Research suggests that the harmful effects of nicotine are at least partially reversible:
- In the large retrospective analysis of 7,680 implants, ex‑smokers who waited more than two years after quitting before undergoing implant surgery had significantly lower failure rates than those who continued to smoke[6]. Patients who underwent implantation within two years of quitting still faced a 2.7‑fold higher failure risk[6], highlighting that the body needs time to recover from tobacco exposure.
- A clinical protocol known as Bain’s protocol recommends that patients stop smoking one week before implant placement and refrain for at least eight weeks afterwards to allow nicotine to clear and new blood vessels to grow[12]. Adhering to this regimen has been associated with improved implant survival.
- The American Academy of Implant Dentistry advises smokers to quit two weeks before surgery and remain smoke‑free for at least eight weeks afterward[13]. Patients who follow this guideline have demonstrated success rates around 94 %, comparable to non‑smokers, whereas those who kept smoking saw success rates closer to 81 %[13].
- A retrospective analysis of implant failures found that smokers who avoided smoking during the healing period had markedly lower rates of early failure compared with those who smoked continuously[12].
Taken together, these findings suggest that temporary abstinence around the time of surgery may nearly eliminate the additional risk posed by smoking. Longer‑term cessation (beyond two years) provides even better outcomes and aligns implant success rates more closely with those of non‑smokers.
Other factors that influence success
Although smoking plays a significant role, implant survival is multifactorial. Other systemic and local factors also contribute to failure:
- Periodontal disease and oral hygiene: The AAP/AO consensus notes that patients with a history of severe periodontitis, poor plaque control or lack of regular maintenance therapy are at higher risk for peri‑implant mucositis and peri‑implantitis[9]. Good oral hygiene and professional maintenance visits are therefore critical.
- Diabetes and metabolic conditions: Uncontrolled diabetes can impede wound healing and increase susceptibility to infection. The AAP/AO report found diabetes mellitus significantly associated with peri‑implantitis (OR 2.31)[10]. Obesity and metabolic syndrome are also moderate risk factors for mucositis[9].
- Bone quality and implant site: Implants placed in the upper jaw (maxilla) tend to have slightly higher failure rates due to less dense bone. In smokers, the hazard of implant loss in the maxilla was 5.64 times higher[1]. Adequate bone volume and density (through grafting if necessary) improve outcomes.
- Medication use: Some drugs, such as proton pump inhibitors, antidepressants and bisphosphonates, have been linked to slightly higher implant failure rates due to altered bone metabolism and healing【981】.
- Surgical skill and prosthetic design: Proper implant placement and prosthetic design minimize overloading and improve cleaning access. Misaligned or malpositioned implants dramatically increase peri‑implantitis risk (odds ratio up to 48 for malpositioned implants)[14].
Despite the influence of these factors, smoking remains one of the most modifiable risks. Professional organizations like the AAP and AO explicitly recommend considering smoking status when planning implant treatment and providing cessation support[15].
Real‑world perspectives: dentists and patients
Dr. Maria Santos, a periodontist in Lisbon, recalls one memorable case. “Paulo came in with three failed implants,” she says. “He had been smoking a pack a day for over twenty years. Each time, the implant would heal initially but start loosening within a few years. After the third failure, he finally quit smoking. When we placed the new implants, we insisted he stay smoke‑free for at least two months. Those implants have now been stable for five years.”
Paulo’s story illustrates a common pattern: persistent smokers often experience repeated implant failure, while those who quit - even temporarily - give their bodies a chance to heal properly. Dentists face a delicate balance. They want to help patients restore their smiles, but they also must set realistic expectations. Many clinicians now incorporate smoking cessation programs into implant treatment. As one practitioner noted, “We’re not here to judge - we’re here to help patients achieve the best possible outcome. If that means delaying surgery until you’re ready to quit, it’s worth it.”
At the same time, not all smokers will experience failure. Genetics, oral hygiene and bone quality vary. Some light or occasional smokers may have successful implants for many years, while some non‑smokers with uncontrolled diabetes or poor hygiene may face complications. Dentists therefore individualize risk assessment, taking into account a patient’s overall health, medications, and commitment to maintenance.
Practical steps for smokers considering implants
How to tilt the odds in your favor
If you’re a smoker thinking about dental implants, the data might feel discouraging. But there are concrete steps you can take to improve your chances of success:
- Quit or cut back before surgery. Ideally, stop smoking two to four weeks before implant placement and stay smoke‑free for at least eight weeks afterward[13][12]. This allows blood vessels to recover and new bone to form.
- Plan for temporary alternatives. Ask your dentist if using nicotine patches or lozenges during the cessation period is appropriate. Avoid smoking alternatives like vaping or chewing tobacco, which can still impair healing.
- Maintain excellent oral hygiene. Brush and floss diligently, and use antibacterial mouth rinses as recommended. Schedule regular cleanings and follow‑up visits to monitor healing.
- Control systemic conditions. Work with your physician to manage diabetes, hypertension or other health issues. Maintain a balanced diet rich in calcium and vitamin D to support bone health.
- Discuss implant options. Some implant systems have surfaces designed to improve osseointegration or designs that minimize bone stress. Your dentist may also recommend bone grafting or soft‑tissue augmentation to optimize the implant site.
- Stay engaged in long‑term maintenance. Even after successful osseointegration, regular dental visits are crucial. Peri‑implantitis often develops years later and is more common in smokers[9].
By following these strategies and working closely with your dental team, you can significantly reduce the risks associated with smoking.
The bottom line: is it worth stubbing out that last cigarette?
Dental implants are one of the most successful treatments in modern dentistry, with survival rates exceeding 90 % in non‑smokers. But smokers face a steeper climb: success rates drop to roughly 80-85 %, failure odds double or triple, and heavy smoking can reduce long‑term survival to around 77 %[5]. Smoking also heightens the risk of peri‑implantitis, bone loss and implant loss over time[10].
The good news is that quitting or even temporarily abstaining can markedly improve outcomes. Patients who stopped smoking weeks before surgery and remained abstinent during healing achieved success rates close to 94 %[13]. The longer you stay smoke‑free, the closer your risk approximates that of a non‑smoker[6].
Ultimately, dental implant success depends on both your dentist’s skill and your own choices. Smoking is one of the few factors you can control. If you’re considering implants, talk openly with your dentist about your smoking status, develop a cessation plan, and commit to rigorous oral hygiene. As research shows, your smile may depend not just on titanium and bone, but on your willingness to stub out that last cigarette.
[1] [3] The Long-Term Effect of Smoking on 10 Years’ Survival and Success of Dental Implants: A Prospective Analysis of 453 Implants in a Non-University Setting - PMC
https://pmc.ncbi.nlm.nih.gov/articles/PMC7230390/
[2] Smoking and Dental Implants: A Systematic Review and Meta-Analysis - PMC
https://pmc.ncbi.nlm.nih.gov/articles/PMC8780868/
[4] [5] The Effects of Smoking on Dental Implant Failure: A Current Literature Update - PMC
https://pmc.ncbi.nlm.nih.gov/articles/PMC11506801/
[6] The effect of cigarette smoking habits on the outcome of dental implant treatment - PMC
https://pmc.ncbi.nlm.nih.gov/articles/PMC4157230/
[7] Quitting Smoking Can Decrease Your Risk of Implant Failures | Dentist in Green Cove Springs
[8] Factors Affecting Dental Implant Failure: A Retrospective Analysis - PMC
https://pmc.ncbi.nlm.nih.gov/articles/PMC12193482/
[9] [10] [11] [14] [15] AO/AAP consensus on prevention and management of peri‐implant diseases and conditions: Summary report - PMC
https://pmc.ncbi.nlm.nih.gov/articles/PMC12273748/
[12] Smoking and dental implants - PMC
https://pmc.ncbi.nlm.nih.gov/articles/PMC3894084/
[13] How Does Smoking Affect the Success of Dental Implants?
https://connect.aaid-implant.org/blog/smoking-dental-implants
